QF-PCR Testing
Quantitative Fluorescence-Polymerase Chain Reaction Testing

Prenatal Diagnosis with QF-PCR: Advanced Genetic Testing
QF-PCR is a molecular biology technique used to diagnose chromosomal abnormalities from fetal amniotic cells. This test can detect several syndromes, including:
- Down Syndrome (Trisomy 21)
- Patau Syndrome (Trisomy 13)
- Edwards Syndrome (Trisomy 18)
- Sex chromosome Aneuploidies (Klinefelter Syndrome, Turner Syndrome)
When to Get Tested with QF-PCR
- .Double/Triple/Quadruple Marker Test Results
When tests indicate the fetus is at risk of birth defects..
- .Double/Triple/Quadruple Marker Test Results
When tests indicate the fetus is at risk of birth defects..
- Maternal Age & Genetic History
Pregnant women over 35 years old due to the higher risk of fetal malformations also History of pregnancies or childbirth with genetic conditions.
Advantages of QF-PCR
- Rapid & Cost Effective
- Can Identify Mosaicism & Maternal Cell Contamination
- Common Aneuploidies Can Be Detected
- Zygosity
- Robust & Confirmatory Test
Result in as little as 24 hrs
Atleast 10% of mosaic and maternal cell contamination can be identified
Detection of common trisomies, sex chromosome aneuploidy and triploidy.
QF-PCR can tell us if it is a singleton or a twin pregnancy.
Cope with poor quality of samples. No further analysis is required..

When to get tested?

Double/Triple/Quadruple Marker Test Results
When tests indicate the fetus is at risk of birth defects..
Ultrasound Abnormalities
Ultrasound findings with heart defects, gastrointestinal issues, absence of nasal bone or other abnormalities corresponding to common aneuploidies.


Maternal Age & Genetic History
Pregnant women over 35 years old due to the higher risk of fetal malformations also History of pregnancies or childbirth with genetic conditions.
FAQ Frequently Asked Questions
- At Greenarray, QF-PCR is done using blood sample as well as amniocentesis fluid sample.
- Yes, QF-PCR is highly accurate for detecting the specified chromosomal abnormalities. However, it is often used in conjunction with other tests for comprehensive prenatal diagnosis.
- No, QF-PCR specifically targets common aneuploidies of chromosomes 13, 18, 21, X, and Y. It does not detect all genetic disorders or structural chromosome abnormalities.
- There is no special preparation required for the QF-PCR test itself. However, preparing for the procedures to obtain fetal cells (like amniocentesis) will involve consulting with your healthcare provider for specific instructions.
- Results are typically communicated through your healthcare provider, who will explain the findings and discuss any further steps or follow-up testing if necessary
Unlock new ways to track
and boost your baby's health during
pregnancy!

Non-Invasive Prenatal Test- GENERA
"Ensuring Your Baby’s Health, One Simple Test at a Time"
Discover the Future of Prenatal Care with NIPS
Expecting a baby is a journey filled with excitement and anticipation. At Peace of Mind Prenatal, we understand the importance of knowing your baby is healthy. Our Non-Invasive Prenatal Testing (NIPS) offers you the reassurance you need without the risks of traditional invasive procedures.

Who should get tested?
Expecting a baby is a journey filled with excitement and anticipation. At Peace of Mind Prenatal, we understand the importance of knowing your baby is healthy. Our Non-Invasive Prenatal Testing (NIPT) offers you the reassurance you need without the risks of traditional invasive procedures.
NIPS offers valuable insights into your baby’s development and is accessible to all pregnant women, regardless of age. Genera NIPS is recommended for all types of pregnancies.
For physicians, it is important to recommend this test for pregnancies where:
- Any pregnant women above 10 weeks of gestation.
- A high risk for abnormality is found in serum screening.
- Certain abnormalities on ultrasound are identified.
- There is a family history of chromosomal conditions or birth defects.
- Couples have had a child with a chromosomal disorder.
- A couple has a history of infertility or pregnancy loss (miscarriages or stillbirths).


What are the conditioned Genera NIPS detect?
GENERA NIPS
- Trisomy 21 (Down Syndrome)
- Trisomy 18 (Edward’s Syndrome)
- Trisomy 13 (Patau’s Syndrome)
- Turner Syndrome (Monosomy XO)
- Triple X syndrome (Trisomy X)
- Klinefelter syndrome (XXY)
- Jacobs Syndrome (XYY)
Note: Sex of the fetus is not determined/ reported by Greenarray as per PC-PNDT Act, 2003
What does Genera (NIPS) test for?
Genera (NIPS) is a Safe, Accurate, Genetic Evaluation of placental DNA in maternal blood using Next Generation Sequencing technology, to estimate the risk of a fetus having Trisomy 21, Trisomy 18, Trisomy 13, Rare Autosomal Aneuploidies (RAA), Sex Chromosome Aneuploidies (SCA) and the most clinically relevant microdeletions.
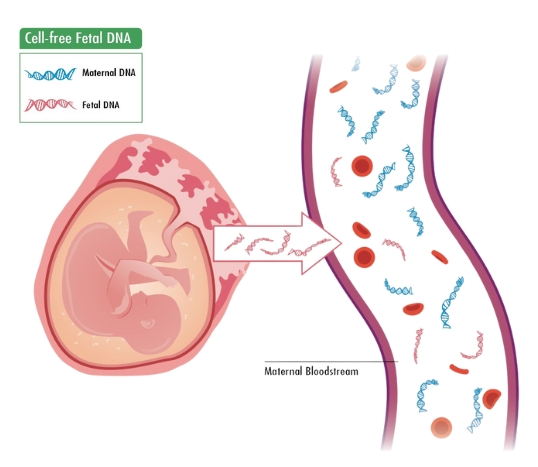
- During pregnancy, the placenta releases small fragments of the baby's genetic material (DNA) into your bloodstream.
- Approximately 2-20% of the total cfDNA in maternal blood is of placental origin.
- Non-Invasive Prenatal Testing (NIPS) analyzes this placental DNA to assess the likelihood of the baby having certain chromosomal abnormalities.
Unique DNA Differentiation
Genera test can distinguish between maternal and fetal DNA, enhancing accuracy.
Early Testing Availability
Can be ordered as early as 9 weeks of pregnancy.
No Risk of Miscarriage
Non- invasive in nature thus reducing the risk of miscarriage therby reducing the need for invasive procedures.
Why Choose
Genera (NIPS)
Superior Test Accuracy
Achieves over 99.9% sensitivity and specificity for Trisomies 21, 18, and 13.
Minimal Test Failures
Ensures a call rate greater than 99%.
images/icons/Comprehensive Fetal Genome Analysis.png
Provides a comprehensive analysis of the entire fetal genome, extending beyond the common trisomies in chromosomes 21, 18, and 13
Rapid Turnaround Time
Delivers results within 7-10 working days.
FAQ Frequently Asked Questions
- NIPS is a simple blood test that analyzes the baby's DNA in the mother's blood, looking for chromosomal abnormalities. It poses no risk to the baby, is 99 percent accurate and can be done as early as 10 weeks.
- If the Fetal Fraction (FF%) in your blood sample is found to be below the standard FF% cut-off of 4% (which occurs in less than 1-2% of cases), you will be asked to provide a repeat blood sample. This repeat sample will be processed at no extra cost.
- Fetal Fraction (FF%) refers to the amount of fetal DNA circulating in the mother's bloodstream, and it varies for each pregnant mother.
- Positive result means that it is likely that your baby will have one of the tested conditions, for example Down syndrome or another. If the result of your non-invasive prenatal test is positive, you should consult with your doctor and plan another diagnostic testing to confirm this result or exclude diagnosis related to that result
- Negative result means that it is unlikely your baby will have Down syndrome or another chromosomal defect analyzed by this non-invasive prenatal test. However, due to technique limitations, a certain subgroup of diseases is not detectable by this test.
- NIPS is a simple blood test that analyzes the baby's DNA in the mother's blood, looking for chromosomal abnormalities. It poses no risk to the baby, is 99 percent accurate and can be done as early as 10 weeks.
- Prenatal test spots genetic anomalies (defects) linked to miscarriage. A blood test can scan a fetus's entire genome (genetic makeup) for chromosomal abnormalities at 10 weeks of pregnancy. NIPS works by detecting DNA fragments from the fetus that are circulating in the maternal blood
- One key risk factor for Down syndrome: maternal age. A 25-year-old woman has a 1 in 830 chance of having a baby with Down syndrome; by 35, the risk has increased to 1 in 350; by age 40, to 1 in 100; and by 49, it's 1 in 10, according to the National Down Syndrome Society.
- You don't need to do anything special to prepare for first trimester screening. You can eat and drink normally before both the blood test and the ultrasound exam.
- Edwards syndrome, also known as trisomy 18, is a genetic disorder caused by a third copy of all or part of chromosome 18. Many parts of the body are affected. Babies are often born small and have heart defects.
- Trisomy 13, also called Patau syndrome, is a chromosomal condition associated with severe intellectual disability and physical abnormalities in many parts of the body.
- Monosomy refers to a single copy of a chromosome. Females with Monosomy X, which is also known as Turner syndrome, are missing a second copy of an X chromosome
- Possible causes of false positive results for trisomy 21 from NIPS include: Confined placental mosaicism (CPM) This is caused by a population of cells in the placenta with three copies of chromosome 21 instead of the usual two. These cells are confined to the placenta and are not present in the baby.
- A low risk NIPS result means that the chance for trisomy 21, trisomy 18 or trisomy 13 is less than 1: 10,000. It does not mean that the chances are zero. It is reassuring but does not guarantee the birth of a baby without any health concerns or other genetic conditions and further tests are recommended.
- When the result is High Risk, confirmatory analysis is suggested after consultation with genetic counsellor or physician. Confirmatory prenatal diagnosis involves amniocentesis or chorionic villus sampling.
- For pricing related questions, kindly contact Greenarray Genomic Research and Solutions directly by calling us at- +91 98230 49121 / 7030024643
Early Detection, Better
Protection – Invest in Your Newborn’s
Future with Greenarray

Newborn Genetic Screening
Rare genetic conditions can lead to severe, chronic, and life-threatening complications. Without newborn genetic screening, these conditions may go undiagnosed or misdiagnosed, posing significant risks to a baby's health and future well-being.
Newborn Screening- Need of the hour!
In India, approximately 2-3% of newborns
are affected by congenital disorders. Remarkably, nearly 70% of these conditions can
be prevented with early detection and intervention. With around 26 million births
annually, the potential impact of undiagnosed genetic disorders is vast.
Early screening is crucial as it allows for timely medical intervention,
significantly improving a child's quality of life and reducing long-term healthcare
costs.
Newborn Genetic Analysis by Greenarray is designed to identify DNA changes that could cause severe or life-altering symptoms in an infant. Our comprehensive analysis includes:
- 258 Genes: A thorough examination of the genetic blueprint.
- Over 400 Disorders: Screening for a wide array of conditions, many of which are beyond the scope of state-legislated standards for newborn screening.
- Greenarray offers a concise yet powerful gene panel, encompassing 47 genes that address 34 critical disorders.
In India, approximately 2-3% of newborns are affected by congenital disorders. Remarkably, nearly 70% of these conditions can be prevented with early detection and intervention. With around 26 million births annually, the potential impact of undiagnosed genetic disorders is vast.
Early screening is crucial as it allows for timely medical intervention, significantly improving a child's quality of life and reducing long-term healthcare costs.
When is the Test Performed?
The test is not time-dependent and can be performed at any time after birth, unlike conventional newborn screening (NBS).
- During pregnancy, the placenta releases small fragments of the baby's genetic material (DNA) into your bloodstream.
- Approximately 2-20% of the total cfDNA in maternal blood is of placental origin.
- Non-Invasive Prenatal Testing (NIPS) analyzes this placental DNA to assess the likelihood of the baby having certain chromosomal abnormalities.

Heel Prick/Dry Blood
Spot
Peripheral Blood
Cord Blood
| Targeted Condition | Disorders | Greenarray’s Newborn Genetic Screening | Conventional NBS |
|---|---|---|---|
| Blood Disorders | Proplonic Acidemia, Phenylketonuria, Medium chain-acyl-CoA dehydrogenase deficiency, Galactosemia, Citrullinema, Argininosuccinic aciduria, Methylmalonic acidemia, Tyrosinemia, Maple- syrup urine disease (MSUD), Homocystinuria, etc. | Yes | Yes |
| Blood Disorders | Thrombocytopenia, hemophilia A, Thalassemia, β- thalassemia, Sickle cell disease, etc. | Yes | No |
| Congenital Hearing Loss | Charcot-Marie-Tooth Disease with deafness, Non-Syndromic hearing loss, Corneal Dystrophy, Perceptive Deafness etc. | Yes | No |
| Immunoddeficiency Disorders(SCID) | Omenn Syndrome, Immunodeficiencies, etc. | Yes | No |
| Congenital heart Defects | Ventricular tachycardia, etc. | Yes | No |
| Neuromuscular Disorder | Spinal Muscular Atrophy, Myopathy, etc. | Yes | No |
| Pediatric Cancers | Xeroderma Pigmentosum, etc. | Yes | No |
| Epilepsy | Seizures, Pyrodixine dependent epilepsy, Seriod Lipofuscinosis, etc. | Yes | No |
| Vision Loss | Retinal Dystrophies, Juvenile Retinoschisis, Retinitis Pigmentosa, etc. | Yes | No |
| Vision Loss | Retinal Dystrophies, Juvenile Retinoschisis, Retinitis Pigmentosa, etc. | Yes | No |
FAQ Frequently Asked Questions
- No, it is not mandatory but is highly recommended to ensure early detection and treatment of potential health issues.
- The test involves a small prick on the heel to collect blood, which may cause brief discomfort, but it is safe and minimally invasive.
- Results are typically available within 2-3 weeks.
- If a disorder is detected, our team will guide you through the next steps, including additional testing, treatment options, and counseling.
- Yes, you can arrange for the test to be done at a healthcare facility or through a home visit by a medical professional.
- Consult your healthcare provider or local health department for detailed information and guidance on newborn genetic screening programs.
Our testing is essential in
helping to diagnose genetic diseases
and explore potential treatment options

Cytogenetics
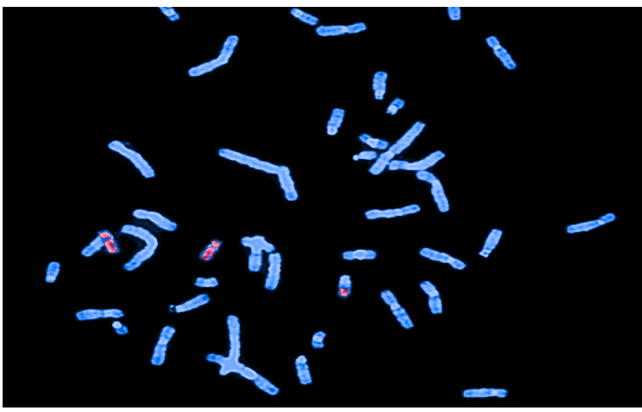
Cytogenetic testing reveals crucial insights into disease progression and treatment response.
By examining blood, amniofluid or Chorionic Villus we detect abnormalities like broken, rearranged, or missing chromosomes. Harnessing karyotyping, FISH, and CGH, cytogenetics scrutinizes chromosomal material for genetic irregularities. These techniques diagnose disorders, predict outcomes, and guide treatments with precision.
When and why is a Karyotype Performed?
- Advanced Maternal Age
- Abnormal Ultrasound Findings
- Previous Pregnancy with Chromosomal Abnormalities
- Unexplained Infertility or Recurrent Miscarriages
- Parental Chromosomal Abnormalities

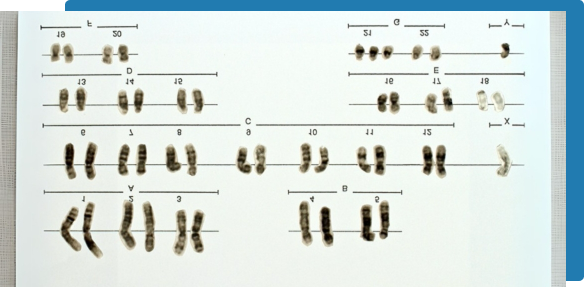
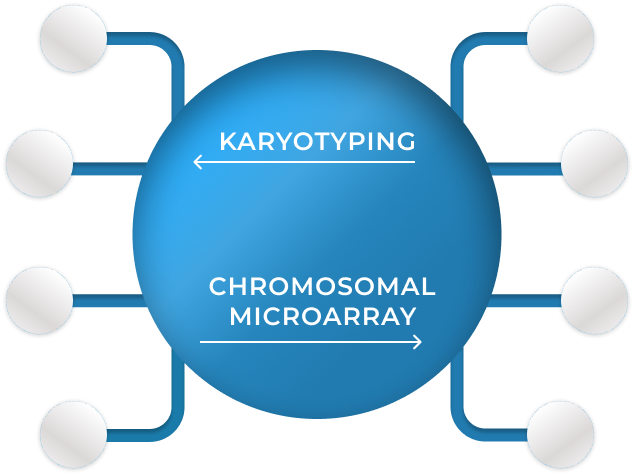
Karyotyping:
Karyotyping is the study to identify chromosomes and look for any gross chromosomal changes such as balanced rearrangements, extra copies/reduced copies of chromosomes
What does it detect?
By examining blood, amniofluid or Chorionic Villus we detect abnormalities like broken, rearranged, or missing chromosomes. Harnessing karyotyping, FISH, and CGH, cytogenetics scrutinizes chromosomal material for genetic irregularities. These techniques diagnose disorders, predict outcomes, and guide treatments with precision.
What does it detect?
- Numerical abnormalities such as trisomies (e.g., Down syndrome, trisomy 18)
- Structural abnormalities like translocations, deletions, and duplications
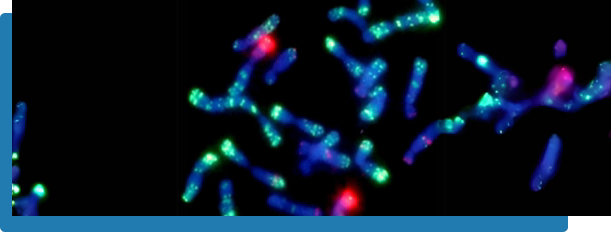
Fluorescence In Situ Hybridization (FISH)
- FISH is a molecular cytogenetic technique that uses fluorescent probes to bind to specific DNA sequences on chromosomes. This allows for the visualization of genetic material in cells.
- The FISH method can detect small changes in chromosomes that conventional cytogenetic methods cannot identify.
- The flourescent signal intensity and localization makes it a quantitative method.


Microdeletions & Duplications-
- Prader-Willi / Angelman syndrome (15q11)
- DiGeorge / VCFS syndrome (22q11 / 10p14)
- Wolf–Hirschhorn syndrome (WHS) (4p-)
- Cri-du-chat syndrome (5p-)
- Williams syndrome (7q11.23)
- Miller – Dieker (MDS) syndrome (17p13.3)
- Smith – Magenis (SMS) syndrome (17p11.2)
Importance of Cytogenetic testing in Prenatal Diagnosis
- Early Detection
- Accurate Diagnosis:
- Informed Planning:
- Risk Assessment:
- Carrier Identification:
- Miscarriage Risk:
Identifies genetic disorders early in pregnancy, enabling informed decision-making.
Get precise information about chromosomal abnormalities, reducing uncertainty and enabling targeted medical care.
Early planning ensures that necessary care, therapies, or surgeries are in place when the baby arrives.
Knowing the likelihood of conditions helps in making informed medical and lifestyle choices.
identify carriers of genetic disorders to make informed reproductive decisions. Options like IVF with genetic screening or adoption can be considered to mitigate risks.
Understand the risk of miscarriages by identifying balanced chromosomal rearrangements in parents.

FAQ Frequently Asked Questions
- No special preparation is needed for this test.
- Cytogenetic testing as such carries minimal to no risk however with respect to sample collection during amniocentesis or CVS Sampling procedure. Proper care and professional expert can minimize the risks.
- CVS sampling is done at 12-13 weeks of pregnancy while amniocentesis is done at16-18 weeks
- Normal result rules out the possibility of having chromosomal abmormality in the fetus.
- Genetic counseling is highly recommended before and after cytogenetic testing. Counselors help you understand the implications of test results, assess risks, and provide support in decision-making.
Think of CMA as your go-to
for uncovering the smallest genetic
clues with precision and clarity!

Chromosomal Microarray
The human body is made up of billions of cells, each containing chromosomes packed with genes. Typically, cells have 46 chromosomes arranged in 23 pairs—half from each parent. The first 22 pairs match up in both sexes, while the 23rd pair determines gender: XX for females and XY for males.
Think of CMA as your go-to for uncovering the smallest genetic clues with precision and clarity!
What is Chromosomal Microarray Analysis?
- Chromosomal Microarray Analysis (CMA), a high-resolution, whole-genome screening known as a molecular karyotype.
- This test uses over 1.9 million copy number probes and about 750,000 SNP probes to spot copy number changes in the chromosome.
- Such findings can guide further testing for imprinting disorders or autosomal recessive diseases.
What does CMA Detect?
- Microdeletions & microduplications of chromosome segments
- Chromosomal Aneuploidy
- Unbalanced translocations and rearrangements
- Intellectual Disability syndromes
When is CMA recommended?
Chromosomal Microarray Analysis is recommended for conditions-
- Developmental and Intellectual Disabilities
- Autism Spectrum Disorders
- Congenital Anomalies
- Unexplained Clinical Syndromes
- Multiple Anomalies
- Prenatal Testing
- Recurrent Pregnancy Loss:
- Infertility
FAQ Frequently Asked Questions
- CMA can only reveal the relative copy-number states of chromosomes and genomic segments, not their location. As such, structural abnormalities generating unbalanced rearrangements can only be inferred from CMA results, and balanced translocations with no associated imbalance are undetectable.
- Ideally, a maternal sample should be submitted concurrently with the products of conception sample. Maternal blood samples are used for maternal cell contamination studies to ensure that the results obtained are reflective of the fetus and not maternal tissues.
- CMA is used to determine if chromosomal abnormalities are present in miscarried fetal tissue, which can provide insights into the cause of the miscarriage and guide future reproductive planning.
- The turnaround time for CMA results can vary but typically ranges from a few days to a few weeks, depending on the laboratory and specific test.
- If CMA reveals an abnormal result, genetic counseling is recommended to interpret the findings and discuss potential implications. Further testing, such as parental CMA or specific gene testing, might be suggested to understand the inheritance pattern and associated risks
- No, CMA is primarily designed to detect CNVs and regions of homozygosity. It does not identify single-gene disorders, balanced translocations, or epigenetic changes. Other genetic tests, such as whole exome sequencing or targeted gene panels, may be required for those conditions
Where Parenthood Begins with Expert Insights.
Genetic Carrier Screening:
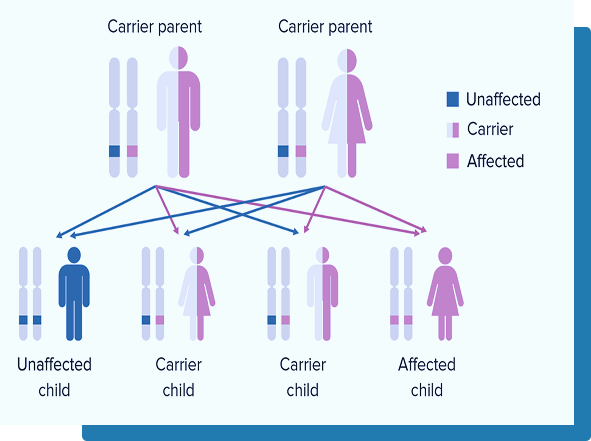
Carrier Genetic Testing (CGT) is an advanced screening test that helps determine whether a couple are carriers of genetic mutations that could be passed on to their children. This test is essential for couples who want to understand potential genetic risks and make informed decisions when planning a family.
What Happens If I'm a Carrier?
Being a carrier of a genetic condition doesn’t mean you will develop the condition yourself. In fact, most people are carriers of one or more genetic conditions and remain healthy. However, if both parents carry a disease-causing variant in the same gene, there is a 25% (1 in 4) chance of having a child affected by that genetic condition
The Importance of Carrier Screening:
Inherited disorders account for approximately 20% of infant mortality in developed countries, underscoring the importance of early genetic screening. Identifying genetic risks before conception allows couples to take proactive steps to reduce the chances of passing on serious conditions to their children.
Greenarray's Carrier Genetic Testing (CGT) provides comprehensive screening, using Next-Generation Sequencing (NGS) to analyze a wide range of inherited disorders, including Cystic Fibrosis, Spinal Muscular Atrophy, Fragile X Syndrome, and Sickle Cell Anemia. Our advanced technology and expert guidance allow families to plan for a healthier future with confidence.
Single Gene Disorders:
Spinal Muscular Atrophy:-
Spinal Muscular Atrophy (SMA) is a rare neuromuscular disorder affecting 1 in 6,000–10,000 births, causing progressive muscle weakness, breathing challenges, and growth issues. About 95–98% of cases are linked to a deletion in the SMN1 gene, vital for muscle function. Its "genetic partner," SMN2, produces limited protein, but the number of SMN2 copies influences disease severity, making genetic testing a critical tool.
Diagnosing SMA: The key to unlocking SMA lies in cutting-edge genetic testing which detects SMN1 and SMN2 deletions, duplications, and copy numbers with over 99% accuracy. Think of it as a molecular detective that reveals the genetic story behind SMA.
Genetic insights are not just for diagnosis—they’re for hope. Testing determines SMN2 copy numbers, guiding therapies that amplify SMN2’s potential to restore muscle function.
Duchene Muscular Dystrophy:-
Duchenne Muscular Dystrophy (DMD) is a prevalent X-linked recessive neuromuscular disorder primarily affecting children. It results from mutations in the DMD gene, preventing the production of functional dystrophin, a critical protein for skeletal muscle contraction.
- Patients exhibiting signs of dystrophinopathy and having elevated levels of serum CK
- Female relatives of men and boys with DMD who wish to assess their disease carrier status
When is the test offered?
The DMD test is recommended for the following conditions:


PGT (Preimplantation Genetic Testing):
PGT-A is a groundbreaking genetic test that analyzes embryo cells to check for the normal number of chromosomes. This advanced screening helps identify embryos with chromosomal abnormalities, paving the way for healthier pregnancies and reducing the risk of miscarriage or failed implantation. Most individuals have 46 chromosomes, inheriting 23 from each parent. However, an unequal division of chromosomes during the formation of sperm or egg cells can result in an embryo having too many or too few chromosomes, a condition called aneuploidy.
Aneuploidy is one of the leading causes of:
- Failed implantation.
- Recurrent miscarriages.
- Birth defects such as Down syndrome, Turner syndrome (trisomy 18), and Patau syndrome (trisomy 13).
Who Should Consider PGT-A?
PGT-A is particularly beneficial for:
- Couples with a history of pregnancies involving aneuploidy.
- Women who have experienced two or more miscarriages.
- Women with unexplained infertility or failed embryo implantation.
- Those undergoing repeated unsuccessful fertility treatments.
CFTR Gene mutation:
Cystic Fibrosis (CF) is a genetic disorder caused by mutations in the CFTR gene (Cystic Fibrosis Transmembrane Conductance Regulator). This gene plays a crucial role in regulating the movement of salt and water in and out of cells. Mutations in CFTR disrupt this balance, leading to thick, sticky mucus buildup in the lungs, pancreas, and other organs.
Who Should Consider CFTR Mutation Testing?
- Individuals with a family history of CF or CFTR-related disorders.
- Couples planning a pregnancy, especially if one or both partners are known carriers.
- Newborns with positive CF newborn screening results.
- Individuals experiencing symptoms such as chronic lung infections, poor growth, or infertility.
A simple blood draw is enough to get to know about your CFTR status!
Our advanced CFTR mutation testing ensures accurate results, empowering individuals and families with actionable knowledge. Whether you’re looking to confirm a diagnosis, assess carrier status, or better understand your genetic health, we’re here to help.

Y Chromosome Microdeletion:
Chromosomes serve as the body's blueprints, with men having one X and one Y chromosome, while women have two X chromosomes, in addition to the 22 pairs of autosomes. In some men, small sections of the Y chromosome may be missing, a condition known as Y chromosome microdeletion. These deletions can disrupt sperm production, making it a significant genetic factor in male infertility.
How Does the Y-Chromosome Microdeletion Test Work?
This test analyzes a blood sample to detect missing segments in the Y chromosome. It identifies genetic factors that may impact fertility, such as low sperm count (oligospermia) or the absence of sperm (azoospermia), providing valuable insights into male infertility.
Who Should Consider the Y-Chromosome Microdeletion Test?
This test is recommended for men facing fertility challenges, including:
- Azoospermia, severe oligozoospermia, or cryptozoospermia (no or very low sperm count).
- Men experiencing unexplained infertility despite trying to conceive.
It offers crucial insights to guide treatment and planning for parenthood.
How to Get a Y-Chromosome Microdeletion Test Done?
To schedule your Y-Chromosome Microdeletion Test, contact
Greenarray Genomics at:
Call +91-9823049121 / 7030024643 or
greenarraylabs@gmail.com
Fragile X Syndrome :
Fragile X Syndrome is a genetic disorder that can cause a range of challenges, including learning difficulties, intellectual disabilities, and behavioral issues. Children with this condition often experience delayed speech and language development, sometimes until after the age of two.
Individuals with Fragile X Syndrome may also exhibit traits of autism spectrum disorder (ASD) or behaviors like anxiety, attention-deficit disorder (ADD), and attention-deficit hyperactivity disorder (ADHD). These complexities can affect communication, social interactions, and daily functioning.
What Causes Fragile X Syndrome?
Fragile X Syndrome occurs due to a mutation in the FMR1 gene on the X chromosome. This mutation involves an excessive repetition of a DNA sequence called the "CGG triplet." Normally, this sequence repeats fewer than 45 times. However:
Premutation: 55–200 repeats, may cause health issues later in life and increase the risk of passing the mutation to children.
Full Mutation: Over 200 repeats, leading to a lack of FMRP protein, essential for brain development.
This deficiency can result in learning difficulties, intellectual disability, and behavioral challenges.
Symptoms are generally milder in females due to the presence of a second X chromosome. Since Fragile X can be inherited even by asymptomatic carriers, women planning a family are advised to check their carrier status before pregnancy.